Maintaining Healthy Peristomal Skin
If the skin around the stoma (peristomal skin) becomes damaged, it could be painful and lead to infection. It also becomes more difficult for the skin barrier of the pouching system to adhere to the skin. Prevention is the key to maintaining both healthy peristomal skin and comfort.
Having a peristomal (around the stoma) skin complication is one of the most common reasons people living with an ostomy seek medical attention. Urine and feces can be irritating to the skin. That’s why a skin barrier or adhesive is essential in preventing peristomal skin damage.
Common Causes of Peristomal Skin Damage
- Leakage: Healthy skin exposed to fecal or urine output under the skin barrier can breakdown fast.1
- Pressure: Belts and some clothing may cause pressure on the stoma area.2
- Stoma size: Ensure the skin barrier is cut to the right size. It should always fit closely around the stoma (1-2mm larger) to protect against leakage.
- Skin folds or creases may prevent the skin barrier from sticking securely to the stomach and result in leakage. A different shaped product may be required if the stoma is flush or retracted.
- Skin stripping or friction by removing a skin barrier too quickly can pull the top layers of skin away. The more frequent it happens, the more the skin can be irritated.3
- Pouching system: If the red or irritated area of the skin is the same shape as the skin barrier, the patient may have developed an allergy or sensitivity.
Tips for Peristomal Skin Care Routine
- Changing the pouch routinely.
- Gently removing the skin barrier from top to bottom – an adhesive remover may help.
- Cleaning the skin around the stoma with a wipe soaked in warm water.
- Using a soap that is oil and residue-free.
- Drying the skin thoroughly before applying the next bag.
- Inspecting the skin with every skin barrier change.
- Applying a skin barrier foam or spray, if needed.
As a general rule, healthy peristomal skin should look the same as skin anywhere else on the body. Often times, when the barrier is removed the patient will notice some redness from the adhesive. That's normal. If the redness does not go away, however, it could be the sign of a peristomal skin issue. Discomfort is another sign that their peristomal skin is not healthy.
Remember: It doesn't take much time or a large amount of effluent touching the peristomal skin for it to be damaged. The damage is not always easy to detect. That's why you should have your patients familiarize themselves with the importance of their peristomal skin, this way, they will know the warning signs and how to manage the skin issue. Ensure your patients receive the support, information and resources they need.
me+™ Program
Enroll your patients in the Convatec Ostomy me+™ support program.
Managing Peristomal Skin Issues
At some point, you may encounter a patient who has unhealthy peristomal skin. Identifying the skin issue is the first step in management. Here are some common peristomal skin issues and general information about them, including description, causes and symptoms.
Candidiasis
Description/Causes: Often caused by leakage, perspiration, antibiotic therapy, warm climates, broken skin.
Symptoms: Itchy, bumpy red skin, infection of vagina, armpit, mouth, or any area of skin folds (i.e., buttocks, groin).

Allergic Contact Dermatitis3
Description/Causes: Often caused by exposure to materials and compounds that irritate or sensitize the skin on contact (e.g., tape, skin barriers, soap, adhesives, powders, pastes, or pouch material).
Symptoms: Redness, itching, broken skin, Irritation in the area covered by a part of the pouching system, a history of allergies.

Irritant Dermatitis2
Description/Causes: Inflammation of peristomal skin resulting from contact with stool or urine, usually from leakage under the pouching system.
Symptoms: Redness, weeping areas of skin.

Pseudoverrucous Lesions (Hyperplasia commonly called PEH)
Description/Causes: Often caused by chronic exposure of the skin to urine due to an excessively large opening in the skin barrier.
Symptoms: Pain Wart-like, gray or purple-colored thickened areas next to the stoma, frequent leakage or bleeding, white, sandy, or gritty granules on stoma or around base.

Folliculitis3
Description/Causes: An inflammation within a hair follicle caused by traumatic hair removal (e.g., "ripping" skin barrier from skin, shaving too closely, or excessive rubbing or cleaning of peristomal skin).
Symptoms: Reddened, pinpoint, or infected areas at the base of the hair follicles around the stoma.
Pressure Ulcer3
Description/Causes: An ulcer in the peristomal area caused by excessive pressure from an ostomy appliance belt, tight clothing, rigid faceplate, peristomal hernia, or work-related habits.
Symptoms: Pain, irregularly shaped ulcer, pouch leakage, decreased wear time.

Psoriasis
Description/Causes: A common skin disorder that can occur underneath ostomy pouching systems.
Symptoms: Whitish scaly patches of various sizes, itching.

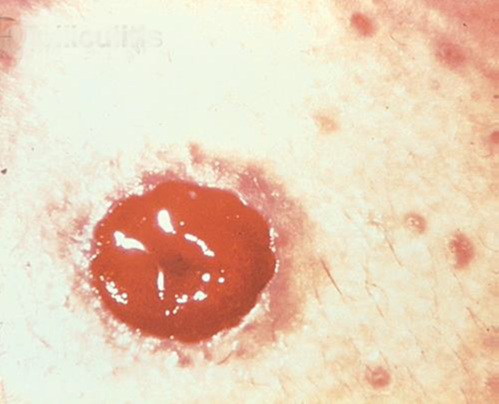
Pyoderma Gangrenosum3
Description/Causes: An inflammatory skin disease often seen in patients with inflammatory bowel disease ( IBD ) such as Crohn's disease or ulcerative colitis.
Symptoms: Irregularly shaped, red, painful, infected ulcers, with red-to-purple rolled margins; appear on legs, buttocks, face, and peristomal area.

Caput Medusae3
Description/Causes: Refers to a bluish-purple discoloration of the skin caused by dilation of the cutaneous veins around the stoma (peristomal varices).
Symptoms: Blue/purple area surrounding the stoma that when blanched, displays irregular, small blood vessels.

More in For Healthcare Professionals
1. Woo KY, Sibbald RG, Ayello EA. Coutts PM. Garde DE. Peristomal Skin Complications and Management. Advances in Skin & Wound Care. 2009; 22(11):522-532.
2. Morss‐Walton PC, Yi J, Gunning, M; McGee JS. Ostomy 101 for dermatologists: Managing peristomal skin diseases. Dermatologic Therapy. 2021; 34(5):1-10.
3. Peristomal Skin Complications Clinical Resource Guide. Wound, Ostomy, and Continence Nurse Society®. 2015.
Give your ostomy patients an invaluable layer of support and care to help them through their recovery after ostomy surgery.
With me+, we surround your patients with the education, support and resources they need to feel stronger, more confident and ready for what's ahead. Our program is designed to guide the right support at the right time at all stages of life.
